Introduction
Maintaining HIPAA compliance on healthcare websites is crucial for protecting PHI (Protected Health Information) and upholding patient privacy. The Health Insurance Portability and Accountability Act (often referred to in short form as HIPAA or the portability and accounting act) was introduced in the United States to address the health insurance portability, security, and accountability requirements within the healthcare industry.
This legislation covers not only insurance portability and accounting but also standards such as the HIPAA Security Rule and the HIPAA Privacy Rule, both of which apply to a wide range of personal data in healthcare settings.
Yet, even well-intentioned organizations often overlook key health IT security principles. The results can be devastating—from PHI leakage to hefty fines for a HIPAA violation. Oversights can lead to cyber attacks, ransomware attacks, and legal scrutiny from the Office for Civil Rights (OCR), the enforcement arm that handles potential breaches of civil rights and patient privacy in healthcare.
In this article, we’ll explore five common HIPAA pitfalls that often result in data breaches on healthcare websites and provide practical steps for PHI safeguarding. We will also delve deeper into how to handle mobile devices, mitigate human error, and take corrective actions in the face of violations. By understanding these pitfalls, you will be better equipped to know how to prevent PHI leakage on healthcare websites.
Pitfall #1: Insecure Data Transmission
When sending sensitive data through website design for healthcare, using data encryption is essential for PHI leakage prevention. Under the HIPAA Security Rule, which focuses on the technical and administrative safeguards required to protect electronic PHI (ePHI), websites must feature secure web forms protected by SSL/TLS certificates.
This ensures that sensitive information such as patient billing details or telehealth data remains confidential and intact during transfer. If data travels unencrypted, it exposes healthcare organizations to cybersecurity threats—like ransomware attacks and other cyber attacks—and often results in HIPAA enforcement actions and fines.
Key Tips
- Always implement HTTPS connections to secure data in transit. This step is fundamental in preventing unauthorized interception of ePHI.
- Employ robust cybersecurity measures such as TLS 1.2 or higher, ensuring strong encryption standards are used.
- Use reputable vendors for healthcare data storage solutions and regularly verify their compliance with insurance portability and accounting standards.
Additionally, consider the use of a Web Application Firewall (WAF) to further reduce the risk of interception or infiltration, particularly important if you handle high volumes of personal data. Monitoring and regularly updating these encryption certificates are critical, especially given evolving security standards in the United States.
Pitfall #2: Poor Access Controls
Even if data is protected during transit, weak access controls can undermine healthcare security best practices. The HIPAA Security Rule requires appropriate administrative and technical safeguards, including limiting data access to authorized personnel only. Human error—such as using weak passwords or failing to deactivate former employees’ accounts—remains a frequent source of PHI leakage. When unauthorized individuals gain entry to protected areas, it leads to significant risk management issues, potential HIPAA audit failures, and the need for costly corrective actions.
Actionable Steps
- Role-based permissions: Grant staff access only to the minimum necessary data to perform their jobs. This aligns with HIPAA’s “minimum necessary” standard.
- Strong authentication: Use multi-factor authentication (MFA) for administrative and clinical accounts, especially for users accessing from mobile devices.
- Regular password rotations: Implement secure password management policies to reduce the likelihood of account compromise.
In addition to these steps, keep a thorough record of role assignments and track any alterations to permissions. Incorporate insurance portability and accounting provisions into your policies, ensuring that employees understand the significance of controlling access to sensitive healthcare data.
Pitfall #3: Insufficient Staff Training
Even the most advanced cybersecurity measures can fail if employees aren’t trained properly. Regular compliance training is key to fostering a culture of patient privacy and accountability. From web administrators to front-desk personnel, every staff member must understand how to handle PHI securely, what the HIPAA Privacy Rule entails, and why abiding by accounting act HIPAA standards is non-negotiable.
Proper training also extends to how employees use mobile devices for work, emphasizing the risk of ransomware attacks and cyber attacks. The civil rights OCR often issues guidance on how to develop and maintain comprehensive staff training programs that address various forms of human error—including accidental disclosure of patient information.
Training Topics
- Recognizing phishing attempts: A common source of data breaches. Make sure staff can spot suspicious emails that could lead to stolen credentials.
- Proper usage of telehealth security solutions and remote communication tools. These platforms must meet HIPAA requirements to ensure personal data is protected.
- Updates on HIPAA compliance regulations and healthcare compliance checklists. Emphasize the interplay between insurance portability and accounting and digital data security obligations.
Encourage staff to stay current on the latest security protocols and to proactively report potential vulnerabilities. This helps transform compliance from a rigid requirement into a shared organizational goal, critical in the healthcare industry where patient trust is paramount.
Pitfall #4: Missing or Outdated Privacy Policies
An accurate and accessible privacy policy is a non-negotiable element of any healthcare website. This policy must reflect compliance with both the HIPAA Privacy Rule—which governs how PHI is used and disclosed—and the HIPAA Security Rule, which prescribes technical safeguards to maintain confidentiality and integrity. Moreover, your privacy policy should explicitly address scenarios involving how to prevent PHI leakage on healthcare websites, referencing best practices in encryption, secure access, and corrective actions procedures if a breach occurs.
Not only is an up-to-date policy a critical part of HIPAA compliance, it also builds trust with patients, who often worry about how their personal data is handled online. Outdated or missing policies raise immediate red flags for regulators during a HIPAA audit, risking fines and reputational damage—issues that can be magnified by negative media coverage or legal consequences in the United States.
How to Stay Compliant
- Frequent Reviews: Audit your privacy and security policies quarterly or whenever changes to your web platform occur. This ensures alignment with any new guidance from the civil rights OCR.
- Easy Access for Users: Make your privacy policy clearly visible, often via a footer link, and ensure it’s updated to reflect real-time changes in PHI safeguarding practices.
- Legal Validation: Consult with healthcare compliance experts or legal counsel for policy verbiage and regulatory requirements. This is particularly important for reflecting portability and accounting act provisions and the complexities of HIPAA.
Pitfall #5: Lack of Ongoing Risk Analysis
Security risk analysis is not a one-off process. Continuous monitoring and evaluation allow you to spot vulnerabilities before they become major HIPAA pitfalls. Routine assessments help maintain robust health IT security and demonstrate adherence to HIPAA enforcement standards. Whether you’re dealing with mobile devices, on-site servers, or cloud-based solutions, a thorough risk analysis will identify weak points in your infrastructure and processes, reducing the risk of PHI leakage and cyber attacks.
Risk Management Steps
- Assess Current Measures: Conduct internal and external security reviews. Evaluate how your staff and systems handle personal data in day-to-day operations.
- Document Findings: Keep a detailed record of vulnerabilities and the measures taken to address them. This documentation is crucial for HIPAA audit readiness and for showing corrective actions.
- Implement Action Plans: Use results from risk analyses to update processes and technology solutions. For instance, if certain user roles require broader access, strengthen your authentication protocols.
- Follow Up: Revisit assessments regularly to verify the effectiveness of newly implemented controls. Ensure your training programs reflect these controls, especially if your organization relies on mobile devices for data handling.
A proactive approach to risk analysis goes hand in hand with the overarching principles of health insurance portability—protecting patient information while enabling efficient healthcare delivery. When done properly, ongoing risk analysis can significantly reduce the likelihood of ransomware attacks and human error leading to inadvertent disclosures.
Additional Considerations for HIPAA Compliance
Beyond these five pitfalls, there are broader aspects of HIPAA and overall healthcare security best practices that your organization should address. By understanding both the HIPAA Security Rule (technical safeguards) and the HIPAA Privacy Rule (use and disclosure of PHI), you’ll be in a stronger position to protect patient data, ensure business continuity, and maintain the trust of your patient population.
- Addressing Mobile Device Security
- Enforce mobile device management (MDM) solutions to ensure remote wiping and encryption capabilities.
- Implement strict policies governing which applications can be installed on company-provided devices.
- Train staff to avoid public Wi-Fi networks or to use Virtual Private Networks (VPNs) when handling PHI.
- Preventing Ransomware Attacks
- Keep all software, including operating systems and antivirus solutions, up to date.
- Regularly back up data and store backups offline or in secure cloud environments to facilitate quick recovery.
- Conduct regular security drills to test staff preparedness in identifying and reporting suspicious emails or system anomalies.
Ransomware attacks are a leading cause of healthcare data breaches worldwide. Attackers often leverage phishing emails or exploit unpatched software vulnerabilities. Once ransomware encrypts your files, you risk losing access to critical patient data, leading to operational downtime and potential HIPAA violations if PHI is compromised.
- Human Error: The Hidden Threat
- Establish a clear organizational culture that emphasizes security first.
- Implement robust access logging to identify any irregular account behavior.
- Provide frequent refresher courses on safe email practices, password hygiene, and the necessity of locking screens.
While sophisticated hacking gets the headlines, human error often plays a larger role in PHI exposures. Employees inadvertently emailing PHI to the wrong address, failing to log out of shared workstations, or neglecting updates to mobile devices can all result in significant breaches.
- Office for Civil Rights (OCR) Enforcement
- Respond promptly and transparently if a breach occurs. OCR will consider your timely notification to affected individuals and proactive containment measures as mitigating factors.
- Keep thorough documentation of all training sessions, risk analyses, and security improvements.
- If an investigation does occur, demonstrate that your organization has adopted the correct administrative, technical, and physical safeguards.
The civil rights OCR is responsible for enforcing HIPAA regulations, investigating breaches, and ensuring that healthcare organizations take corrective actions in response to violations. Penalties can range from issued resolutions requiring changes in policy to large financial settlements.
How to Prevent PHI Leakage on Healthcare Websites
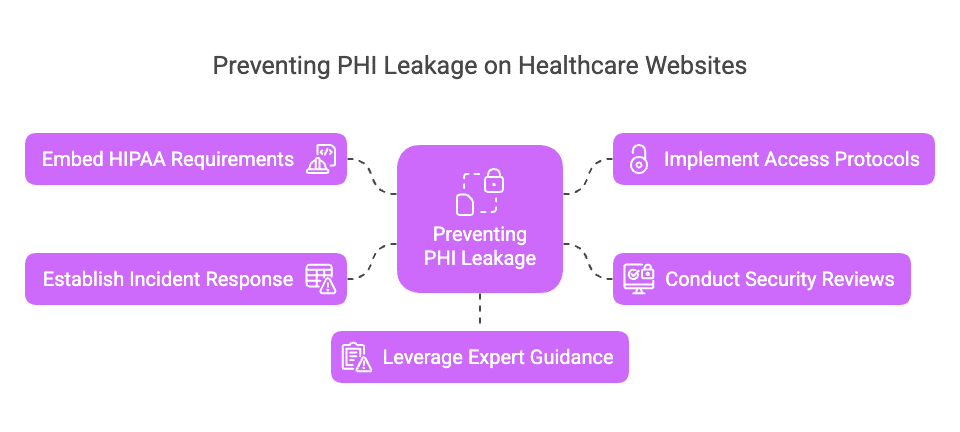
Knowing how to prevent PHI leakage on healthcare websites involves a multi-layered approach that addresses the entire information lifecycle—from data creation and input to storage, access, and final disposal. Here’s a concise roadmap integrating the best practices discussed:
- Embed HIPAA Requirements into Website Architecture
- Integrate SSL/TLS certificates at the outset and configure your content management system (CMS) to enforce HTTPS connections.
- Design forms and databases with the “minimum necessary” principle in mind, collecting only essential PHI.
- Evaluate plugins or third-party integrations for compliance alignment with the portability and accounting act requirements.
- Implement Comprehensive Access and Authentication Protocols
- Use role-based access and MFA for both onsite and remote workers.
- Deploy identity and access management (IAM) tools to track user activities, helping you spot anomalies early.
- Continuously update user permissions to reflect changes in job roles or employment status.
- Conduct Periodic Security Reviews and Staff Training
- Schedule formal risk assessments to adapt to emerging threats like ransomware attacks and advanced cyber attacks.
- Provide scenario-based training on topics like phishing emails, secure device usage, and proper disposal of printed documents.
- Revisit internal policies regularly, ensuring they align with updated federal guidelines in the United States.
- Establish a Robust Incident Response Plan
- Draft a response policy detailing immediate steps upon detection of a breach.
- Assign responsibilities to an incident response team, with clear communication channels to senior management and legal advisors.
- Inform the civil rights OCR if a breach meets the defined threshold, and conduct corrective actions to prevent future incidents.
- Leverage Expert Guidance
- Engage with legal counsel or HIPAA compliance consultants to ensure your policies reflect both the HIPAA Security Rule and the HIPAA Privacy Rule.
- Subscribe to official channels for alerts on new threats, vulnerability disclosures, or regulatory changes in the healthcare industry.
- Stay informed about the interplay between accounting act HIPAA provisions and your day-to-day website operations.
Conclusion and Next Steps
PHI leakage prevention requires vigilance, proper compliance training, and robust cybersecurity measures tailored to healthcare websites. By addressing these five HIPAA pitfalls—from data encryption to continuous risk management—you can build a stronger defense against data breaches and maintain patient privacy. It’s critical to remember that HIPAA is not just about health insurance portability; it also encompasses strict guidelines for securing personal data, whether that’s stored on in-house servers or accessed via mobile devices.
The healthcare industry in the United States faces unique regulatory challenges, making it essential to understand the fine details of the HIPAA Security Rule and the HIPAA Privacy Rule. Implementing the right protocols, training your employees thoroughly, and staying up to date on evolving threats—especially ransomware attacks—will minimize the risk of falling into these pitfalls.
Moreover, demonstrating a commitment to ongoing compliance and corrective actions not only reduces legal exposure but also reinforces trust among your patient base. Healthcare organizations that proactively address these issues are better positioned to handle the complexities of insurance portability and accounting while maintaining integrity and security for all forms of personal data.
Ready to fortify your organization’s health IT security? Start free website assessment to learn more about securing your healthcare platform and safeguarding PHI. For advanced guidance, including a healthcare compliance checklist, consult trusted sources such as the U.S. Department of Health & Human Services. By doing so, you’ll stay informed of any regulatory updates, reinforcing your ability to know exactly how to prevent PHI leakage on healthcare websites and maintain the highest standards of privacy and security in this ever-evolving digital landscape.